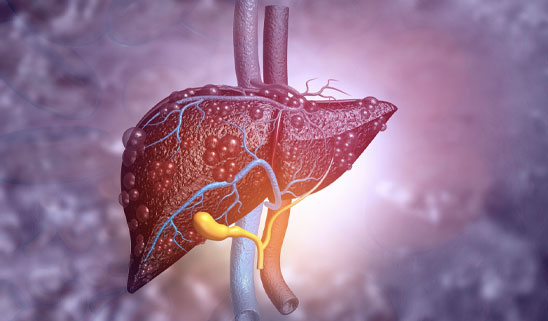
Liver cirrhosis is a condition that affects the liver, the largest organ in the body. The liver performs many vital functions, such as filtering toxins from the blood, producing bile to help digest fats, and making proteins that are essential for blood clotting and other processes. When the liver is damaged by various causes, such as viral infections, alcohol abuse, or fatty liver disease, it tries to heal itself by forming scar tissue. However, too much scar tissue can impair the liver’s ability to function properly and lead to complications such as portal hypertension, bleeding varices, ascites, hepatic encephalopathy, and liver cancer.
Cirrhosis is a serious and potentially life-threatening condition that requires medical attention and treatment. The treatment depends on the cause and stage of cirrhosis, as well as the symptoms and complications that the patient experiences. Some of the common treatments include medications to reduce inflammation and prevent infections, diuretics to remove excess fluid from the body, endoscopic procedures to stop bleeding from enlarged veins in the esophagus or stomach, and liver transplantation for patients with end-stage liver disease.
The best way to prevent cirrhosis is to avoid or treat the factors that can damage the liver. Some of the preventive measures include avoiding alcohol or drinking in moderation, getting vaccinated against hepatitis A and B, practicing safe sex and avoiding sharing needles, maintaining a healthy weight and diet, and taking medications only as prescribed by a doctor.
Stages of liver cirrhosis
The stages of liver cirrhosis are based on the extent of liver damage and the presence or absence of complications. According to the most common classification system, there are four stages of liver cirrhosis:
Stage 1:
This is the earliest stage, where there is inflammation of the liver or bile ducts, but no significant scarring or fibrosis. The liver can still function normally and compensate for the damage. The symptoms are usually mild or absent, and may include abdominal discomfort, fatigue, or loss of appetite. The treatment at this stage is to address the underlying cause of the inflammation, such as viral infection, alcohol abuse, or fatty liver disease.
Stage 2:
This is the stage where scarring or fibrosis starts to develop in the liver due to chronic inflammation. The scar tissue blocks the normal flow of blood and bile in the liver, affecting its function. The symptoms may become more noticeable and include jaundice (yellowing of the skin and eyes), itching, swelling of the legs or abdomen, spider veins on the skin, or easy bruising or bleeding. The treatment at this stage is to slow down the progression of fibrosis and prevent complications, such as portal hypertension (high blood pressure in the vein that carries blood to the liver) or varices (enlarged veins in the esophagus or stomach that can bleed).
Stage 3:
This is the stage where cirrhosis is established, meaning that there is extensive scarring and hardening of the liver tissue. The liver can no longer compensate for the damage and its function is significantly impaired. The symptoms may worsen and include ascites (fluid accumulation in the abdomen), hepatic encephalopathy (confusion, memory loss, or coma due to toxins in the brain), or liver cancer. The treatment at this stage is to manage the symptoms and complications, such as using diuretics (water pills) to reduce fluid retention, endoscopic procedures to stop bleeding from varices, or medications to improve brain function.
Stage 4:
This is the final stage, where liver failure occurs. This means that the liver can no longer perform its vital functions and the patient’s life is in danger. The symptoms may include severe bleeding, infection, kidney failure, or multi-organ failure. The treatment at this stage is to provide supportive care and palliative care, or to consider liver transplantation as a last resort option.
Causes of liver cirrhosis
The causes of liver cirrhosis are various factors or conditions that can damage the liver and lead to scarring and impaired function. According to the web search results, some of the most common causes of liver cirrhosis are:
Alcoholic liver disease: This is the damage to the liver and its function due to alcohol abuse. Alcohol can cause inflammation, fat accumulation, and oxidative stress in the liver, which can lead to fibrosis and cirrhosis over time.
Nonalcoholic fatty liver disease: This is a condition in which fat accumulates in the liver, usually due to obesity, diabetes, or metabolic syndrome. The excess fat can cause inflammation and oxidative stress in the liver, which can lead to fibrosis and cirrhosis over time.
Chronic hepatitis C: This is a viral infection that affects the liver and can cause chronic inflammation and fibrosis. The hepatitis C virus can be transmitted through blood or body fluids, such as by sharing needles, having unprotected sex, or receiving contaminated blood transfusions. The infection can persist for years without symptoms, but can eventually lead to cirrhosis or liver cancer.
Chronic hepatitis B: This is another viral infection that affects the liver and can cause chronic inflammation and fibrosis. The hepatitis B virus can be transmitted through blood or body fluids, such as by sharing needles, having unprotected sex, or from mother to child during birth. The infection can be acute or chronic, and can lead to cirrhosis or liver cancer if not treated.
Some of the less common causes of liver cirrhosis include:
Autoimmune hepatitis: This is a liver disease in which the immune system attacks the liver cells, causing inflammation and damage. The exact cause of autoimmune hepatitis is unknown, but it may be triggered by genetic factors, environmental factors, or infections. Autoimmune hepatitis can be treated with immunosuppressive drugs, but may progress to cirrhosis if left untreated.
Bile duct diseases: These are diseases that damage, destroy, or block the bile ducts, which are tubes that carry bile from the liver to the gallbladder and intestine. Bile is a fluid that helps digest fats and remove toxins from the body. Some examples of bile duct diseases are primary biliary cholangitis and primary sclerosing cholangitis, which are autoimmune disorders that cause inflammation and scarring of the bile ducts . Bile duct diseases can lead to cirrhosis by causing bile backup and liver damage .
Inherited liver diseases: These are diseases passed from parents to children through genes that affect how the liver works. Some examples of inherited liver diseases are Wilson disease, hemochromatosis, and alpha-1-antitrypsin deficiency. Wilson disease causes abnormal accumulation of copper in the body, hemochromatosis causes abnormal accumulation of iron in the body, and alpha-1-antitrypsin deficiency causes abnormal production of a protein that protects the lungs from damage. All these diseases can cause cirrhosis by damaging the liver cells with excess metals or proteins .
Risk of Liver Cirrhosis
The risk of death after liver cirrhosis depends on several factors, such as the cause, stage, and complications of the disease. According to the web search results, some of the common causes of sudden death in patients with liver cirrhosis are:
Massive bleeding from varices: Varices are enlarged veins that develop in the esophagus or stomach due to high blood pressure in the portal vein, which carries blood from the digestive organs to the liver. When these veins rupture, they can cause severe and life-threatening bleeding that requires emergency treatment.
Cardiac death: Patients with liver cirrhosis are at higher risk of developing heart diseases, such as heart attacks and arrhythmias, which can cause sudden death. This may be due to the impaired function of the liver in regulating blood clotting, inflammation, and metabolism.
Hepatic encephalopathy: This is a condition in which toxins accumulate in the brain due to liver failure, causing confusion, memory loss, coma, and death. Hepatic encephalopathy can be triggered by various factors, such as infections, bleeding, medications, or dietary changes.
Liver cancer: Patients with liver cirrhosis have an increased risk of developing liver cancer, which can grow rapidly and spread to other organs. Liver cancer can cause symptoms such as abdominal pain, weight loss, jaundice, and ascites (fluid accumulation in the abdomen). Liver cancer can also cause sudden death due to bleeding or organ failure.
Liver failure: This is the final stage of liver cirrhosis, where the liver can no longer perform its vital functions and the patient’s life is in danger. Liver failure can cause symptoms such as bleeding, infection, kidney failure, or multi-organ failure. Liver failure can also cause sudden death due to shock or sepsis (a severe infection that affects the whole body).
The life expectancy of patients with liver cirrhosis varies depending on the stage and severity of the disease. There are two stages of liver cirrhosis: compensated and decompensated. Compensated cirrhosis means that the liver can still function normally and compensate for the damage. Decompensated cirrhosis means that the liver function is significantly impaired and symptoms and complications occur.
One of the most common classification systems for liver cirrhosis is the Child-Turcotte-Pugh (CTP) system, which assigns points based on five criteria: ascites, hepatic encephalopathy, albumin level, bilirubin level, and prothrombin time (a measure of blood clotting). Based on these points, patients are classified into three classes: A (5-6 points), B (7-9 points), and C (10-15 points)3.
According to one study4, the median survival time for patients with compensated cirrhosis was 12 years for class A, 9 years for class B, and 7 years for class C. The median survival time for patients with decompensated cirrhosis was 2 years for class A, 1 year for class B, and 3 months for class C.
Signs of Liver Cirrhosis
The early signs of liver cirrhosis may vary depending on the cause and stage of the disease. However, some of the common early signs of liver cirrhosis are:
- Fatigue and weakness: You may feel tired and weak due to the reduced function of your liver, which affects your metabolism and energy levels123.
- Loss of appetite and weight loss: You may lose your appetite and weight due to the inflammation and damage in your liver, which affects your digestion and nutrient absorption123.
- Nausea and vomiting: You may feel nauseous and vomit due to the accumulation of toxins in your body, which your liver cannot filter out properly123.
- Upper abdominal pain: You may experience pain or discomfort in your upper right abdomen due to the enlargement or swelling of your liver, which puts pressure on the surrounding organs123.
These early signs of liver cirrhosis are often mild or absent, especially in the initial stages of the disease. As the disease progresses, you may develop more serious symptoms and complications, such as:
- Jaundice: This is a yellowing of your skin and eyes due to the buildup of bilirubin, a pigment produced by your liver when it breaks down red blood cells.
- Itching: This is caused by the accumulation of bile salts, which are substances that help digest fats, in your skin.
- Swelling: This is caused by fluid retention in your legs, feet, ankles, or abdomen (ascites) due to portal hypertension, which is high blood pressure in the vein that carries blood from your digestive organs to your liver.
- Redness on the palms of your hands: This is caused by increased blood flow to your hands due to hormonal changes or vasodilation, which is widening of blood vessels.
- Spider-like blood vessels on your skin: These are small red or purple spots with tiny branches that resemble spider webs. They are caused by increased blood flow to your skin due to hormonal changes or vasodilation.